https://www.mdpi.com/2075-4418/13/2/252
Visual Snow Initiative (VSI) and Misdiagnosis Association and Research Institution (MARI) team up to promote VSS awareness to the international medical community and healthcare professionals…
Age- and frequency-dependent changes in dynamic contrast perception in visual snow syndrome
https://pubmed.ncbi.nlm.nih.gov/34895130/
https://thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-021-01355-y
Age- and frequency-dependent changes in dynamic contrast perception in visual snow syndrome
VSI: Mayo Clinic Acknowledges Visual Snow Syndrome — “Mayo Clinic Minute: Visual Snow”
Mayo Clinic Joins the Cause, Now Acknowledges Visual Snow Syndrome! — “Mayo Clinic Minute: Visual Snow”
https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-minute-visual-snow/
Mayo Clinic Minute: Visual snow
https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-minute-visual-snow/
Mayo Clinic Minute: Visual snow
Visual snow: Alarming and not uncommon
https://www.mdedge.com/psychiatry/article/249122/headache-migraine/visual-snow-alarming-and-not-uncommon
Distinct Patterns of P1 and C2 VEP Potentiation and Attenuation in Visual Snow: A Case Report
https://www.frontiersin.org/articles/10.3389/fneur.2021.723677/full
VisualSnowStudies – Reddit
https://www.reddit.com/r/VisualSnowStudies/
VisualSnowStudies – Reddit
Evaluation of treatment response and symptom progression in 400 patients with visual snow syndrome
https://bjo.bmj.com/content/early/2021/10/20/bjophthalmol-2020-318653
Evaluation of treatment response and symptom progression in 400 patients with visual snow syndrome
Visual Snow Syndrome as a Network Disorder: A Systematic Review
https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC8521005/
Visual Snow Syndrome as a Network Disorder: A Systematic Review
Short-Wave Sensitive (“Blue”) Cone Activation Is an Aggravating Factor for Visual Snow Symptoms
https://www.frontiersin.org/articles/10.3389/fneur.2021.697923/full
Short-Wave Sensitive (“Blue”) Cone Activation Is an Aggravating Factor for Visual Snow Symptoms
Localised increase in regional cerebral perfusion in patients with visual snow syndrome
Localised increase in regional cerebral perfusion in patients with visual snow syndrome
July 14, 2021
https://jnnp.bmj.com/content/early/2021/07/13/jnnp-2020-325881
University of Colorado Researchers Initiate Clinical Trial of Transcranial Magnetic Stimulation for Visual Snow Syndrome
https://clinicaltrials.gov/ct2/show/NCT04925232
Transcranial Magnetic Stimulation For Visual Snow Syndrome
https://clinicaltrials.gov/ct2/show/NCT04925232?cond=Visual+Snow&lupd_s=05%2F31%2F2021&lupd_d=14
Transcranial Magnetic Stimulation For Visual Snow Syndrome
Condition : Visual Snow Syndrome
Intervention : Device: Transcranial Magnetic Stimulation device
Sponsor : University of Colorado, Denver
Recruiting
Mon, 14 Jun 2021 12:00:00 EDT
Visual Snow-Like Symptoms and Posterior Uveitis following COVID-19 Infection
https://pubmed.ncbi.nlm.nih.gov/34123447/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210614150933&v=2.14.4
TITLE:
Visual Snow-Like Symptoms and Posterior Uveitis following COVID-19 Infection
DESCRIPTION:
Visual snow (VS) is a neurologic condition consisting of a constant positive visual disturbance described as “static” with diagnosis requiring exclusion of competing neurologic and ophthalmologic disorders. The authors describe the first case of visual snow-like symptoms in a patient following coronavirus disease 2019 (COVID-19) infection. He was found to have a transient subtle mild inflammatory reaction in the vitreous and optic nerve edema which resolved, but the VS persisted. Our findings…
PMID:
pubmed:34123447
DATE FOUND:
06/14/21 03:09PM
LINK / URL:
https://pubmed.ncbi.nlm.nih.gov/34123447/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210614150933&v=2.14.4
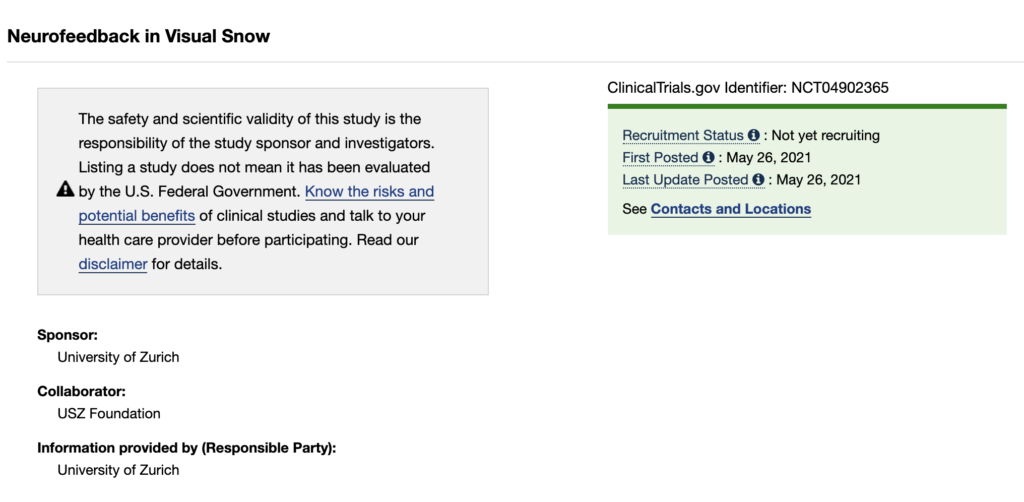
Neurofeedback in Visual Snow
https://clinicaltrials.gov/ct2/show/NCT04902365?cond=Visual+Snow&lupd_s=05%2F12%2F2021&lupd_d=14
Neurofeedback in Visual Snow
Conditions : Visual Snow Syndrome; Neuro-Ophthalmology
Intervention : Other: neurofeedback (based on real-time functional magentic resonance signals)
Sponsors : University of Zurich; USZ Foundation
Not yet recruiting
Wed, 26 May 2021 12:00:00 EDT
Researchers in Switzerland Initiate Clinical Trial for Downregulating Visual Cortex Activity in Visual Snow Syndrome
Some good news:
A new clinical trial for visual snow syndrome was added to the clinicaltrials.gov database earlier today.
 This is the second ever VS study added to the system. But unlike the first study we covered, this one has nothing to do with mindfulness and cognitive behavioral therapy.
This is the second ever VS study added to the system. But unlike the first study we covered, this one has nothing to do with mindfulness and cognitive behavioral therapy.
Instead it focuses on giving patients a way to reduce the actual visual snow intensity and prevalence.
The study is titled, “Neurofeedback for Patients With Visual Snow” and it is expected to start in just over a month from now, on July 1, 2021. Currently not yet recruiting, but that status should change soon.
A total of 70 participants will be enrolled.
The study is taking place at the University of Zurich. It is funded by the USZ Foundation.
In a double-blind, randomized and placebo-controlled longitudinal experiment, we will use real-time functional magnetic resonance imaging (rtfMRI) neurofeedback to teach patients to downregulate activity in different regions of the visual cortex
Here is a brief summary, from the study description:
Visual snow (VS) is a distressing, life-impacting condition with unrelenting and persistent disturbing visual phenomena. Disease onset is usually around age 20 and is characterized by continuous perception of innumerable flickering dots (like a ‘broken television’). The disease is often accompanied by comorbidities such as migraine, tinnitus, depression and anxiety.
Neuronally, VS patients show cerebral hypermetabolism, resulting in altered neuronal excitability, as well as increased grey matter volume in parts of the visual cortex.
For this pilot study, we aim to recruit VS patients. In a double-blind, randomized and placebo-controlled longitudinal experiment, we will use real-time functional magnetic resonance imaging (rtfMRI) neurofeedback to teach patients to downregulate activity in different regions of the visual cortex.
We hypothesize that neurofeedback will allow patients to learn to downregulate their abnormal visual cortex activity. Moreover, we predict a stronger downregulation of activity from the lingual gyrus will correlate with a more pronounced decrease in VS symptoms.
Here is a link to the official study record:
https://clinicaltrials.gov/ct2/show/NCT04902365
That’s all for now.
Important:
This article is an early draft. You are able to access it because you (or someone who shared this link) is subscribed to Visual Snow Treatment Report email updates. Not subscribed? Sign up here. It’s free. Expect between 1-2 emails per week. But only if something new is happening. No spam, no promotional emails. Only goodies like this. Your information is kept private and never shared with third parties.
Already subscribed? Tell a friend or share this article if you know anyone who might find it helpful.
Questions? Feedback? Comments? Send an email to michael@urgentresearch.com and say hello.
A case of visual snow treated with phenylephrine
https://pubmed.ncbi.nlm.nih.gov/34021593/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210522152708&v=2.14.4
TITLE:
A case of visual snow treated with phenylephrine
DESCRIPTION:
No abstract
PMID:
pubmed:34021593
DATE FOUND:
05/22/21 03:27PM
LINK / URL:
https://pubmed.ncbi.nlm.nih.gov/34021593/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210522152708&v=2.14.4
Cortical Oscillatory Dysrhythmias in Visual Snow Syndrome: A MEG Study
https://www.biorxiv.org/content/10.1101/2021.05.17.444460v1
Cortical Oscillatory Dysrhythmias in Visual Snow Syndrome: A MEG Study
Migraine prevalence in visual snow with prior illicit drug use (Hallucinogen Persisting Perception Disorder) versus without
https://pubmed.ncbi.nlm.nih.gov/33979006/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210512200942&v=2.14.4
TITLE:
Migraine prevalence in visual snow with prior illicit drug use (Hallucinogen Persisting Perception Disorder) versus without
DESCRIPTION:
CONCLUSIONS: While none of the HPPD participants had migraine, over half of the visual snow controls without prior use of illicit drugs had migraine. This suggests that at least partly different pathophysiological factors play a role in both disorders. Users of ecstasy and other hallucinogens should be warned of the risk of visual snow. Further studies are needed to enhance understanding of the underlying neurobiology of HPPD and VSS to come to better management of these conditions.
PMID:
pubmed:33979006
DATE FOUND:
05/12/21 08:09PM
LINK / URL:
https://pubmed.ncbi.nlm.nih.gov/33979006/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210512200942&v=2.14.4
White matter abnormalities in a patient with Visual Snow syndrome: new evidence from a Diffusion tensor imaging study
https://pubmed.ncbi.nlm.nih.gov/33960084/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210507140529&v=2.14.4
TITLE:
White matter abnormalities in a patient with Visual Snow syndrome: new evidence from a Diffusion tensor imaging study
DESCRIPTION:
CONCLUSION: This VSS patient displayed multiple, bilateral white matter changes in the temporo-parieto-occipital junction in white matter pathways related to vision. We encourage the study of white matter pathology using DTI in complex neurological syndromes including VSS.
PMID:
pubmed:33960084
DATE FOUND:
05/07/21 02:05PM
LINK / URL:
https://pubmed.ncbi.nlm.nih.gov/33960084/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210507140529&v=2.14.4
Eye movement characteristics provide an objective measure of visual processing changes in patients with visual snow syndrome
https://www.nature.com/articles/s41598-021-88788-2
https://www.nature.com/articles/s41598-021-88788-2
Eye movement characteristics provide an objective measure of visual processing changes in patients with visual snow syndrome
Emma J. Solly, Meaghan Clough, Allison M. McKendrick, Paige Foletta, Owen B. White & Joanne Fielding
Visual snow syndrome – a pixelated vision [German Language]
https://pubmed.ncbi.nlm.nih.gov/33950282/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210505202030&v=2.14.4
TITLE:
Visual snow syndrome – a pixelated vision
DESCRIPTION:
No abstract
PMID:
pubmed:33950282
DATE FOUND:
05/05/21 08:20PM
LINK / URL:
https://pubmed.ncbi.nlm.nih.gov/33950282/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210505202030&v=2.14.4
Magnetic Suppression of Perceptual Accuracy Is Not Reduced in Visual Snow Syndrome
https://pubmed.ncbi.nlm.nih.gov/34017304/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210521190437&v=2.14.4
TITLE:
Magnetic Suppression of Perceptual Accuracy Is Not Reduced in Visual Snow Syndrome
DESCRIPTION:
Objective: Patients with visual snow syndrome (VSS) suffer from continuous (“TV snow-like”) visual disturbance of unknown pathoetiology. In VSS, changes in cortical excitability in the primary visual cortex and the visual association cortex are discussed, with recent imaging studies tending to point to higher-order visual areas. Migraine, especially migraine with aura, is a common comorbidity. In chronic migraine and episodic migraine with aura but not in episodic migraine without aura, a…
PMID:
pubmed:34017304
DATE FOUND:
05/21/21 07:04PM
LINK / URL:
https://pubmed.ncbi.nlm.nih.gov/34017304/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210521190437&v=2.14.4
Dr. Owen White answers the question: “What excites you the most about visual snow research in 2021?” [video]
Visual snow syndrome: evolving neuro-optometric interventions
https://pubmed.ncbi.nlm.nih.gov/34084555/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210604141423&v=2.14.4
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8162163/
TITLE:
Visual snow syndrome: evolving neuro-optometric considerations in concussion/mild traumatic brain injury
DESCRIPTION:
No abstract
PMID:
pubmed:34084555
DATE FOUND:
06/04/21 02:14PM
LINK / URL:
https://pubmed.ncbi.nlm.nih.gov/34084555/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210604141423&v=2.14.4
A message from Dr. Charles Shidlofsky to the Visual Snow Community [video]
In this video, Dr. Charles Shidlofsky answers the question: Is there anything you would like to share with the VSS community?
Not All That Flickers Is Snow
https://pubmed.ncbi.nlm.nih.gov/32235228/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210223145155&v=2.14.2
TITLE:
Not All That Flickers Is Snow
DESCRIPTION:
A woman presented with bilateral visual disturbances that had been diagnosed as visual snow. Dilated ophthalmic examination and multimodal imaging were strongly suggestive of birdshot chorioretinopathy, meriting initiation of systemic immunomodulatory therapy. Visual snow requires a thorough ophthalmologic exam to exclude other ocular diseases.
PMID:
pubmed:32235228
DATE FOUND:
02/23/21 02:53PM
LINK / URL:
https://pubmed.ncbi.nlm.nih.gov/32235228/?utm_source=Other&utm_medium=rss&utm_campaign=None&utm_content=14czX-i9THTbCLiShSwLmfPkYONZQXBzqdieEHoJtKGcAAzgP4&fc=None&ff=20210223145155&v=2.14.2
Two hundred and forty-eight cases of visual snow: A review of potential inciting events and contributing comorbidities
https://www.ncbi.nlm.nih.gov/pubmed/33615842?dopt=Abstract
TITLE:
Two hundred and forty-eight cases of visual snow: A review of potential inciting events and contributing comorbidities.
DESCRIPTION:
Related Articles
Two hundred and forty-eight cases of visual snow: A review of potential inciting events and contributing comorbidities.
Cephalalgia. 2021 Feb 20;:333102421996355
Authors: Mehta DG, Garza I, Robertson CE
Abstract
OBJECTIVE: To review characteristics and outcomes of all cases of visual snow seen at our institution, with attention to possible triggering events or comorbidities.
METHODS: This is a retrospective case series of patients seen at our tertiary care center from January 1994 to January 2020. Charts were reviewed if they contained the term “visual snow”.
RESULTS: Of the 449 charts reviewed, 248 patients described seeing visual snow in part or all of their vision. Thirty-eight reported transient visual snow as their typical migraine aura. Of the remaining 210 patients, 89 were reported to have either an inciting event or contributing comorbidity for their visual snow symptoms, including: Post-concussion (n = 15), dramatic change in migraine or aura (n = 14), post-infection (n = 13), hallucinogen persisting perception disorder (n = 10), ocular abnormalities (n = 7), idiopathic intracranial hypertension (n = 4), neoplastic (n = 1), and posterior cortical atrophy (n = 1). Some patients had partial improvement with benzodiazepines (n = 6), lamotrigine (n = 5), topiramate (n = 3) and acetazolamide (n = 3). Presenting characteristics were similar, but patients with visual snow attributed to an inciting event or contributing comorbidity were more likely to have some improvement in their symptoms by last follow-up compared to spontaneous visual snow (p < .001). CONCLUSIONS: Though most cases of visual snow are spontaneous, potential secondary causes should be recognized by clinicians. Patients who develop visual snow after an inciting event or related to an underlying comorbidity may have a better prognosis than those in whom it develops spontaneously. In select cases, treatment of the suspected underlying cause may significantly alleviate the otherwise typical intractable visual disturbances associated with visual snow. PMID: 33615842 [PubMed - as supplied by publisher] PMID: PubMed:33615842 DATE FOUND: 02/23/21 06:00AM LINK / URL: https://www.ncbi.nlm.nih.gov/pubmed/33615842?dopt=Abstract
Passive visual stimulation induces fatigue or improvement depending on cognitive load [Preprint]
https://www.biorxiv.org/content/10.1101/2020.11.19.390096v2.full
Passive visual stimulation induces fatigue or improvement depending on cognitive load
View ORCID ProfileStefano Ioannucci, Guillermo Borragán, Alexandre Zénon
doi: https://doi.org/10.1101/2020.11.19.390096
Reddit User Creates Open-Source “VS Relief Overlay” App That *Might* Help Improve Visual Snow Symptoms
Disrupted connectivity within visual, attentional and salience networks in the visual snow syndrome
https://www.ncbi.nlm.nih.gov/pubmed/33448525?dopt=Abstract
https://onlinelibrary.wiley.com/doi/10.1002/hbm.25343
TITLE:
Disrupted connectivity within visual, attentional and salience networks in the visual snow syndrome.
DESCRIPTION:
Related Articles
Disrupted connectivity within visual, attentional and salience networks in the visual snow syndrome.
Hum Brain Mapp. 2021 Jan 15;:
Authors: Puledda F, O’Daly O, Schankin C, Ffytche D, Williams SC, Goadsby PJ
Abstract
Here we investigate brain functional connectivity in patients with visual snow syndrome (VSS). Our main objective was to understand more about the underlying pathophysiology of this neurological syndrome. Twenty-four patients with VSS and an equal number of gender and age-matched healthy volunteers attended MRI sessions in which whole-brain maps of functional connectivity were acquired under two conditions: at rest while watching a blank screen and during a visual paradigm consisting of a visual-snow like stimulus. Eight unilateral seed regions were selected a priori based on previous observations and hypotheses; four seeds were placed in key anatomical areas of the visual pathways and the remaining were derived from a pre-existing functional analysis. The between-group analysis showed that patients with VSS had hyper and hypoconnectivity between key visual areas and the rest of the brain, both in the resting state and during a visual stimulation, compared with controls. We found altered connectivity internally within the visual network; between the thalamus/basal ganglia and the lingual gyrus; between the visual motion network and both the default mode and attentional networks. Further, patients with VSS presented decreased connectivity during external sensory input within the salience network, and between V5 and precuneus. Our results suggest that VSS is characterised by a widespread disturbance in the functional connectivity of several brain systems. This dysfunction involves the pre-cortical and cortical visual pathways, the visual motion network, the attentional networks and finally the salience network; further, it represents evidence of ongoing alterations both at rest and during visual stimulus processing.
PMID: 33448525 [PubMed – as supplied by publisher]
PMID:
PubMed:33448525
DATE FOUND:
01/16/21 06:00AM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/33448525?dopt=Abstract
Occipital ischaemic stroke after visual snow phenomenon – a case report
https://pubmed.ncbi.nlm.nih.gov/33435707/
Occipital ischaemic stroke after visual snow phenomenon – a case report
Breakthrough In Diagnosing VSS
Breakthrough In Diagnosing VSS
Nov 25, 2020 | Research
Abnormal Connectivity and Brain Structure in Patients With Visual Snow
https://www.ncbi.nlm.nih.gov/pubmed/33328934?dopt=Abstract
TITLE:
Abnormal Connectivity and Brain Structure in Patients With Visual Snow.
DESCRIPTION:
Related Articles
Abnormal Connectivity and Brain Structure in Patients With Visual Snow.
Front Hum Neurosci. 2020;14:582031
Authors: Aldusary N, Traber GL, Freund P, Fierz FC, Weber KP, Baeshen A, Alghamdi J, Saliju B, Pazahr S, Mazloum R, Alshehri F, Landau K, Kollias S, Piccirelli M, Michels L
Abstract
Objective: Visual snow (VS) is a distressing, life-impacting condition with persistent visual phenomena. VS patients show cerebral hypermetabolism within the visual cortex, resulting in altered neuronal excitability. We hypothesized to see disease-dependent alterations in functional connectivity and gray matter volume (GMV) in regions associated with visual perception.
Methods: Nineteen patients with VS and 16 sex- and age-matched controls were recruited. Functional magnetic resonance imaging (fMRI) was applied to examine resting-state functional connectivity (rsFC). Volume changes were assessed by means of voxel-based morphometry (VBM). Finally, we assessed associations between MRI indices and clinical parameters.
Results: Patients with VS showed hyperconnectivity between extrastriate visual and inferior temporal brain regions and also between prefrontal and parietal (angular cortex) brain regions (p < 0.05, corrected for age and migraine occurrence). In addition, patients showed increased GMV in the right lingual gyrus (p < 0.05 corrected). Symptom duration positively correlated with GMV in both lingual gyri (p < 0.01 corrected). Conclusion: This study found VS to be associated with both functional and structural changes in the early and higher visual cortex, as well as the temporal cortex. These brain regions are involved in visual processing, memory, spatial attention, and cognitive control. We conclude that VS is not just confined to the visual system and that both functional and structural changes arise in VS patients, be it as an epiphenomenon or a direct contributor to the pathomechanism of VS. These in vivo neuroimaging biomarkers may hold potential as objective outcome measures of this so far purely subjective condition. PMID: 33328934 [PubMed] PMID: PubMed:33328934 DATE FOUND: 12/18/20 06:03AM LINK / URL: https://www.ncbi.nlm.nih.gov/pubmed/33328934?dopt=Abstract
Rhythmic modulation of visual perception by continuous rhythmic auditory stimulation [Preprint]
https://www.biorxiv.org/content/10.1101/2020.10.30.362467v1
Rhythmic modulation of visual perception by continuous rhythmic auditory stimulation
Sierra Domb and Dr Peter Goadsby discuss “Visual Snow and Tinnitus: Phantom Phenomena” – via Tinnitus Talk [PDF]
https://www.tinnitustalk.com/podcast/wp-content/uploads/2020/10/transcript-tinnitus-talk-podcast-ep-14-visual-snow.pdf
Visual Snow and Tinnitus — Phantom Phenomena
The two conditions are eerily similar: visual snow and tinnitus. The patient experience is often one of being misunderstood, and research is in its infancy. What can be done? Two pioneers in this field, patient advocate Sierra Domb and neurologist Dr Peter Goadsby, talk about their incredible experiences in trying to push the envelope for visual snow sufferers.
Visual Snow Initiative Funding of the MBCT-Vision Study at St. Thomas’ London
Visual Snow Initiative’s Funding of the MBCT-Vision Study at St. Thomas’ London
Visual Snow Initiative Funding of the MBCT-Vision Study at St. Thomas’ London
Neuro-ophthalmologic Findings in Visual Snow Syndrome
https://thejcn.com/DOIx.php?id=10.3988/jcn.2020.16.4.646
https://www.ncbi.nlm.nih.gov/pubmed/33029971?dopt=Abstract
TITLE:
Neuro-ophthalmologic Findings in Visual Snow Syndrome.
DESCRIPTION:
Neuro-ophthalmologic Findings in Visual Snow Syndrome.
J Clin Neurol. 2020 Oct;16(4):646-652
Authors: Yoo YJ, Yang HK, Choi JY, Kim JS, Hwang JM
Abstract
BACKGROUND AND PURPOSE: The findings of ophthalmic examinations have not been systematically investigated in visual snow syndrome. This study reviewed the abnormal neuro-ophthalmologic findings in a patient cohort with symptoms of visual snow syndrome.
METHODS: We retrospectively reviewed 28 patients who were referred for symptoms of visual snow to a tertiary referral hospital from November 2016 to October 2019. We defined the findings of best corrected visual acuity (BCVA), visual field testing, pupillary light reflex, contrast sensitivity, full-field and multifocal electroretinography, and optical coherence tomography.
RESULTS: Twenty patients (71%) were finally diagnosed as visual snow syndrome. Their additional visual symptoms included illusionary palinopsia (61%), enhanced entoptic phenomenon (65%), disturbance of night vision (44%), and photophobia (65%). A history of migraine was identified in ten patients (50%). The mean BCVA was less than 0.1 logarithm of the minimum angle of resolution, and electrophysiology showed normal retinal function in all patients. Contrast sensitivity was decreased in two of the seven patients tested. Medical treatment was applied to five patients which all turned out to be ineffective. Among the eight patients who were excluded, one was diagnosed with rod-cone dystrophy and another with idiopathic intracranial hypertension.
CONCLUSIONS: Neuro-ophthalmologic findings are mostly normal in patients with visual snow syndrome. Retinal or neurological diseases must be excluded as possible causes of visual snow.
PMID: 33029971 [PubMed]
PMID:
PubMed:33029971
DATE FOUND:
10/09/20 06:02AM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/33029971?dopt=Abstract
Visual snow syndrome after start of citalopram-novel insights into underlying pathophysiology
https://link.springer.com/article/10.1007%2Fs00228-020-02996-9
https://www.ncbi.nlm.nih.gov/pubmed/32939564?dopt=Abstract
TITLE:
Visual snow syndrome after start of citalopram-novel insights into underlying pathophysiology.
DESCRIPTION:
Related Articles
Visual snow syndrome after start of citalopram-novel insights into underlying pathophysiology.
Eur J Clin Pharmacol. 2020 Sep 16;:
Authors: Eren OE, Schöberl F, Schankin CJ, Straube A
PMID: 32939564 [PubMed – as supplied by publisher]
PMID:
PubMed:32939564
DATE FOUND:
09/18/20 06:01AM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/32939564?dopt=Abstract
University student creates nonprofit to support research on Visual Snow Syndrome
https://news.miami.edu/stories/2020/09/university-student-creates-nonprofit-to-support-research-on-visual-snow-syndrome.html?fbclid=IwAR0x0XG3F4SUyNAYn8kWlZtAp97h9DU_tyEGb_CPrm899gIogEVT7SKecoM
University student creates nonprofit to support research on Visual Snow Syndrome
Discovery of “behavioral signature” in visual snow syndrome could pave way for targeted treatments…
https://www.monash.edu/medicine/news/latest/2020-articles/visual-snow-causes-being-revealed
First evidence of quantifiable behavioral changes in visual snow syndrome
Behavioral signature of VSS
Visual snow causes being revealed
By JULIA VEITCH 10 September 2020
A/Prof Jo Fielding explains the research. See video
Neuroscientists have recently characterised how visual processing is disrupted in the condition known as Visual Snow Syndrome (VSS).
Senior author A/Prof Fielding said, “The ocular motor network and its processing of visual information is complex, involving a number of distinct steps that allow us to make sense of how we see the world.”
She said that the network includes areas of the brain involved in sending visual information from the eyes to the brain. It then puts together this visual information using cognitive processes to make a cohesive image, resulting in an eye movement.
“Our study provides the first evidence of objective and quantifiable behavioural changes in patients with visual snow syndrome.”
The team discovered that patients with VSS moved their eyes faster than healthy patients towards a suddenly appearing stimulus. In addition, when asked instead to stop that action and move their eyes in the opposite direction, VSS patients were more likely to erroneously move their eyes towards the stimuli.
Interestingly, when the difficulty of each of these tasks increased, therefore requiring increased demands on an individual’s higher order visual processing in the brain, the results were no different. The patients with VSS still responded with faster eye movements and the proportion of erroneous eye movements did not change.
A/Prof Fielding said, “These results suggest that in people with VSS the visual processing changes are not a consequence of disruption to decision-making centres of the brain. Rather, patients with VSS appear to be processing visual stimuli faster than healthy people, leading to hyper-accelerated eye movements.
“This analysis has provided an essential first step into defining a behavioural signature of VSS, and identifying the brain areas and processes affected.
“Once we know what’s causing the issue, that information can be used to develop targeted treatment and better management of this debilitating syndrome.”
Reference: Emma J Solly, Meaghan Clough, Allison M McKendrick, Paige Foletta, Owen B White, Joanne Fielding. Ocular motor measures of visual processing changes in visual snow syndrome. Neurology. First published July 16, 2020, DOI: https://doi.org/10.1212/WNL.0000000000010372
Video: https://youtu.be/mylkdmppdAM
New October 2020 Visual Snow Study Announced: Tsang/Shidlofsky Working on Enhanced Protocol to Treat VSS
New Oct. 2020 Study Announced, Two Physicians Working On Enhanced Protocol to Treat VSS + Potential Conference
New October 2020 Visual Snow Study Announced: Two Physicians Working On Enhanced Protocol to Treat VSS + Potential Conference…
UPDATE: Visual Snow Initiative releases more video interviews with world’s leading visual snow experts…
https://www.youtube.com/c/VisualSnowInitiative/videos
UPDATE: Visual Snow Initiative releases more video interviews with world’s leading visual snow experts…
Visual snow researcher at Monash University invites people with visual snow to participate in newest VSS study…
Visual snow researcher at Monash University invites people with visual snow to participate in newest VSS study…
PARTICIPATE: Visual Snow Research Team at Monash University asks people with visual snow to complete an online survey for new VSS study
Abnormal visual processing within the ventral visual stream may play a role in the pathogenesis of visual snow syndrome, study finds
https://pubmed.ncbi.nlm.nih.gov/32791921/
Time-dependent branching processes: a model of oscillating neuronal avalanches
https://www.nature.com/articles/s41598-020-69705-5
Time-dependent branching processes: a model of oscillating neuronal avalanches
Johannes Pausch, Rosalba Garcia-Millan & Gunnar Pruessner
Scientific Reports volume 10, Article number: 13678 (2020)
[123I]-IMP single-photon emission computed tomography imaging in visual snow syndrome: A case series
https://journals.sagepub.com/doi/10.1177/0333102420950454
https://www.ncbi.nlm.nih.gov/pubmed/32791921?dopt=Abstract
TITLE:
[123I]-IMP single-photon emission computed tomography imaging in visual snow syndrome: A case series.
DESCRIPTION:
Related Articles
Cephalalgia. 2020 Aug 13;:333102420950454
Authors: Shibata M, Tsutsumi K, Iwabuchi Y, Kameyama M, Takizawa T, Nakahara T, Fujiwara H, Jinzaki M, Nakahara J, Dodick DW
Abstract
BACKGROUND: Visual snow syndrome (VSS) is a neurological condition characterized by persistent flickering dots in the visual fields, palinopsia, enhanced entoptic phenomenon, photophobia, and nyctalopia. Neuroimaging evidence supports the role of the visual association cortex in visual snow syndrome.Case series: We provided clinical care to three patients with visual snow syndrome, in whom [123I]-IMP single-photon emission computed tomography (SPECT) imaging was performed. Case 1 was a 21-year-old male with a past history of migraine with aura who exhibited visual snow and entoptic phenomenon. In this patient, [123I]-IMP SPECT imaging revealed right occipital and temporal hypoperfusion with a distribution matching the ventral visual stream. [123I]-IMP SPECT imaging detected only mild bilateral frontal hypoperfusion in Case 2 and no overt abnormalities in Case 3.
CONCLUSION: Although visual snow syndrome seems to be a heterogenous condition, our observations indicate that abnormal visual processing within the ventral visual stream may play a role in the pathogenesis of this condition.
PMID: 32791921 [PubMed – as supplied by publisher]
PMID:
PubMed:32791921
DATE FOUND:
08/15/20 06:02AM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/32791921?dopt=Abstract
Occipital cortex and cerebellum grey matter changes in visual snow syndrome
https://n.neurology.org/content/early/2020/08/05/WNL.0000000000010530
https://www.ncbi.nlm.nih.gov/pubmed/32759201?dopt=Abstract
TITLE:
Occipital cortex and cerebellum grey matter changes in visual snow syndrome.
DESCRIPTION:
Related Articles
Occipital cortex and cerebellum grey matter changes in visual snow syndrome.
Neurology. 2020 Aug 05;:
Authors: Puledda F, Bruchhage M, O’Daly O, Ffytche D, Williams SCR, Goadsby PJ
Abstract
OBJECTIVE: To determine whether regional grey and white matter differences characterize the brain of patients with visual snow syndrome, a newly defined neurologic condition, we used a voxel-based morphometry approach.
METHODS: In order to investigate directly whole brain morphology, we performed a magnetic resonance imaging study on patients (n = 24) with visual snow syndrome and on age- and gender matched (n = 24) healthy volunteers. Voxel-based morphometry was used to determine volumetric differences in visual snow subjects. We further analysed cerebellar anatomy directly using the high-resolution spatially unbiased atlas template of the cerebellum.
RESULTS: Compared to healthy controls, patients with visual snow syndrome had increased grey matter volume in the left primary and secondary visual cortices, the left visual motion area V5 and the left cerebellar crus I/lobule VI area. These anatomical alterations could not be explained by clinical features of the condition.
CONCLUSION: We conclude that patients with visual snow syndrome have subtle, yet significant neuroanatomical differences in key visual and lateral cerebellar areas, which may in part explain the pathophysiologic basis of the disorder.
PMID: 32759201 [PubMed – as supplied by publisher]
PMID:
PubMed:32759201
DATE FOUND:
08/08/20 06:00AM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/32759201?dopt=Abstract
Ocular motor measures of visual processing changes in visual snow syndrome
https://n.neurology.org/content/early/2020/07/16/WNL.0000000000010372
https://www.ncbi.nlm.nih.gov/pubmed/32675081?dopt=Abstract
TITLE:
Ocular motor measures of visual processing changes in visual snow syndrome.
DESCRIPTION:
Related Articles
Ocular motor measures of visual processing changes in visual snow syndrome.
Neurology. 2020 Jul 16;:
Authors: Solly EJ, Clough M, McKendrick AM, Foletta P, White OB, Fielding J
Abstract
OBJECTIVE: To determine whether changes to cortical processing of visual information can be objectively evaluated using three simple ocular motor tasks to measure performance in patients with visual snow syndrome (VSS).
METHODS: Sixty four patients with VSS (32 with migraine and 32 with no migraine), and 23 controls participated. Three ocular motor tasks were included: prosaccade (PS), antisaccade (AS), and interleaved antisaccade-prosaccade (AS-PS) tasks. All these tasks have been used extensively in both neurologically healthy and diseased states.
RESULTS: We demonstrated that, compared to controls, the VSS group generated significantly shortened PS latencies (p = .029) and an increased rate of AS errors (p = .001), irrespective of the demands placed on visual processing (i.e., task context). Switch costs, a feature of the AS-PS task, were comparable across groups, and a significant correlation was found between shortened PS latencies and increased AS error rates for VSS patients (r = .404).
CONCLUSION: We identified objective and quantifiable measures of visual processing changes in patients with VSS. The absence of any additional switch cost on the AS-PS task in VSS suggests that the PS latency and AS error differences are attributable to a speeded PS response rather than to impaired executive processes more commonly implicated in poorer AS performance. We propose that this combination of latency and error deficits, in conjunction with intact switching performance will provide a VS behavioural signature that contributes to our understanding of VSS and may assist in determining the efficacy of therapeutic interventions.
PMID: 32675081 [PubMed – as supplied by publisher]
PMID:
PubMed:32675081
DATE FOUND:
07/18/20 06:03AM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/32675081?dopt=Abstract
Visual snow syndrome: is it normal or a disorder – and what to do with patients?
https://onlinelibrary.wiley.com/doi/abs/10.1111/ene.14436
https://www.ncbi.nlm.nih.gov/pubmed/32652792?dopt=Abstract
TITLE:
Visual snow syndrome: is it normal or a disorder – and what to do with patients?
DESCRIPTION:
Visual snow syndrome: is it normal or a disorder – and what to do with patients?
Eur J Neurol. 2020 Jul 11;:
Authors: Schankin CJ, Puledda F, Goadsby PJ
Abstract
Recently in the journal, epidemiological data are presented on visual snow syndrome (VSS) using a crowdsourcing online platform [1]. The authors applied criteria for VSS to a sample of people matched for age, sex, and ethnicity to United Kingdom census data. Further, they assessed frequent headache lasting longer than 4 hours, which was interpreted as migraine, and neurological symptoms during headache, interpreted as aura.
PMID: 32652792 [PubMed – as supplied by publisher]
PMID:
PubMed:32652792
DATE FOUND:
07/12/20 06:03AM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/32652792?dopt=Abstract
Multiple Events May Trigger Visual Snow
https://journals.lww.com/neurotodayonline/blog/neurologytodayconferencereporteramericanheadachesocietyannualmeeting/pages/post.aspx?PostID=36
Multiple Events May Trigger Visual Snow
AT THE MEETINGS
HEADACHE/FACIAL PAIN
By Ed Susman
June 30, 2020
Email
Facebook
Twitter
Comment
Visual snow, a mostly spontaneous phenomenon that may be related to migraine, appears to be triggered by inciting events, systemic illness, or lesions along the visual pathway, researchers reported at the virtual annual scientific meeting of the American Headache Society.
Mindfulness Based Cognitive Therapy Modified for Visual Symptoms (MBCT-vision)
https://clinicaltrials.gov/ct2/show/NCT04184726
Insights into pathophysiology and treatment of visual snow syndrome: A systematic review
https://www.sciencedirect.com/science/article/pii/S0079612320300625?via%3Dihub
Insights into pathophysiology and treatment of visual snow syndrome: A systematic review
Author links open overlay panelOzanErenaChristoph J.Schankinb
a
Department of Neurology, LMU Munich, University Hospital—Großhadern, Munich, Germany
b
Department of Neurology, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland
Received 4 March 2020, Revised 25 April 2020, Accepted 1 May 2020, Available online 15 June 2020.
Visual Snow Case Series: Review of 248 Cases with Attention to Underlying Causes or Inciting Events [PDF]
https://3002a505d4f8666b1f13-6d0524d9c8a5052ce15209ae3ecb39a3.ssl.cf1.rackcdn.com//1331558-1590516001.pdf
https://headachejournal.onlinelibrary.wiley.com/doi/abs/10.1111/head.13893
Visual Snow Case Series: Review of 248 Cases with Attention to Underlying Causes or Inciting Events
Noninvasive Vagal Nerve Stimulation in a Pediatric Patient with Visual Snow Syndrome [PDF]
Noninvasive Vagal Nerve Stimulation in a Pediatric Patient with Visual Snow Syndrome.
https://www.eventscribe.com/2020/AHSAnnual/fsPopup.asp?efp=WUJOWk9YWEsxMDkwMg&PosterID=273309&rnd=0.318007&mode=posterinfo
https://3002a505d4f8666b1f13-6d0524d9c8a5052ce15209ae3ecb39a3.ssl.cf1.rackcdn.com//1331552-1590438434.pdf
Visual snow patients show functional hyperconnectivity and structural abnormalities of brain regions involved in visual processing
Ghislaine L Traber; Njoud Aldusary; Patrick Freund; Fabienne C. Fierz; Konrad P Weber; Marco Piccirelli; Arvwa Baeshen; Jamaan Alghamdi; Bujar Saliju; Shila Pazahr; R Mazloum; Fahad Alshehri; Klara Landau; Spyros Kollias; Lars Michels
OPEN ACCESS
Investigative Ophthalmology & Visual Science June 2020, Vol.61, 3387.
Abstract
Purpose: Visual snow (VS) is a distressing, life-impacting condition with persistent visual phenomena. Visual snow patients show cerebral hypermetabolism within the visual cortex, resulting in altered neuronal excitability. We hypothesize to see disease-dependent change in functional connectivity and grey matter in regions associated with visual perception.
Methods: We studied 19 patients with VS and 16 age-matched healthy controls. Functional magnetic resonance imaging (fMRI) was applied to examine resting-state functional connectivity (rsFC). Volume changes were assessed by means of voxel-based morphometry. Finally, we assessed associations between MRI and clinical parameters.
Results: Patients with VS showed significant hyperconnectivity between visual and inferior temporal brain regions, and also between prefrontal, parietal, and cerebellar brain regions (corrected for age and migraine occurrence). In addition, patients showed increased grey matter volume in the lingual gyrus (all p<0.05 corrected). Symptom duration positively correlated to grey matter volume of the bilateral lingual gyrus (p<0.05 corrected).
Conclusions: Our data suggests that VS is associated with abnormal excitability of brain regions involved in visual processing. We conclude that both functional and structural plasticity contributes to evolving impairments in VS patients. These in-vivo neuroimaging biomarkers hold potential to predict individual outcomes and to track the effects of therapeutic intervention.
This is a 2020 ARVO Annual Meeting abstract.
Ghislaine L Traber, Njoud Aldusary, Patrick Freund, Fabienne C. Fierz, Konrad P Weber, Marco Piccirelli, Arvwa Baeshen, Jamaan Alghamdi, Bujar Saliju, Shila Pazahr, R Mazloum, Fahad Alshehri, Klara Landau, Spyros Kollias, Lars Michels; Visual snow patients show functional hyperconnectivity and structural abnormalities of brain regions involved in visual processing. Invest. Ophthalmol. Vis. Sci. 2020;61(7):3387.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Visual Snow: A Case Series from Israel
https://www.karger.com/Article/FullText/508602
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7315196/
https://www.ncbi.nlm.nih.gov/pubmed/32595484?dopt=Abstract
TITLE:
Visual Snow: A Case Series from Israel.
DESCRIPTION:
Related Articles
Visual Snow: A Case Series from Israel.
Case Rep Ophthalmol. 2020 May-Aug;11(2):205-211
Authors: Berkowitz E, River Y, Digre K, Tiosano B, Kesler A
Abstract
Our aim was to examine the symptoms and clinical characteristics of visual snow in a group of 6 patients from a Department of Ophthalmology and a Department of Neurology. Visual snow is now recognized as a true physiological disorder. Previously, physicians unaware of this syndrome may have misinterpreted its symptoms as a persistent visual aura. By promoting awareness of this syndrome, greater quantitative and qualitative research may expand our understanding and treatment of this disorder.
PMID: 32595484 [PubMed]
PMID:
PubMed:32595484
DATE FOUND:
07/01/20 06:05AM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/32595484?dopt=Abstract
Can repetitive transcranial magnetic stimulation of the visual cortex ameliorate the state of patients with visual snow?
https://www.ncbi.nlm.nih.gov/pubmed/32484702?dopt=Abstract
http://www.elis.sk/download_file.php?product_id=6723&session_id=k7qlip0cob6t4s0ua6flkl0rt0
http://www.elis.sk/index.php?page=shop.product_details&flypage=flypage.tpl&product_id=6723&category_id=158&option=com_virtuemart&vmcchk=1&Itemid=1
TITLE:
Can repetitive transcranial magnetic stimulation of the visual cortex ameliorate the state of patients with visual snow?
DESCRIPTION:
Can repetitive transcranial magnetic stimulation of the visual cortex ameliorate the state of patients with visual snow?
Bratisl Lek Listy. 2020;121(6):395-399
Authors: Grey V, Klobusiakova P, Minks E
Abstract
AIMS: Visual snow is a neurological condition, for which an effective treatment has not been established. The aim of this study was to find whether Repetitive Transcranial Magnetic Stimulation (rTMS) can improve the state of patients suffering from visual snow. To our knowledge, no other group has tested this method in the treatment of visual snow.
METHODS: We applied rTMS of 10 and 10+1 Hz on the visual cortices of 9 patients with visual snow. Sham stimulation with the vertex as the target site was also tested. As a method of assessment, we used visual evoked potentials, questionnaires and visual snow diaries. For data evaluation, we used the Paired Sample T-test separately for each stimulation type.
RESULTS: The Paired Sample T-test revealed a decreased sum of visual snow intensities extracted from visual snow diaries in the week after 10+1 Hz stimulation as compared to the figure in the week before (p=0.02).
CONCLUSION: We detected a trend indicating an improvement of patients’ condition based on the data from visual snow diaries. Research on a larger group of patients is required to confirm these findings; however, our study provides a framework to build upon (Tab. 4, Fig. 1, Ref. 22).
PMID: 32484702 [PubMed – as supplied by publisher]
PMID:
PubMed:32484702
DATE FOUND:
06/03/20 06:00AM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/32484702?dopt=Abstract
Natural course of Visual Snow Syndrome: a long-term follow-up study
M. Graber, P.J. Goadsby, A. Scutelnic, C. Schankin
EPR1103
ePresentation Sessions | 162
2020 European Journal of Neurology, 27 (Suppl. 1 (Suppl. 1), 103–522
Abstract
Background and aims: Visual Snow Syndrome (VSS) is characterized by a continuous positive pan-field visual disturbance resembling the view of a badly-tuned analogue television plus associated visual symptoms. For many patients VSS can be disabling. We present the 1st longitudinal study describing the long-term natural course of the disorder over 8 years.
Methods: In total 78 Patients with confirmed VSS, including normal ophthalmologic exams, were followed from November 2011 to December 2019. The clinical course of the disorder was assessed in a semi-structured telephone interview.
Results: 40 of 78 (51%) patients were reached for the follow up interview. Mean follow up time was 83.6±4.5 months. 2 of 40 (5%) reported the onset of additional visual symptoms, which were tunnel vision and light flashes. Compared to 2011, less patients rated visual snow itself as the most disturbing symptom (40% in 2019 vs 72.5% in 2011, p=0.001); instead, patients suffered more from floaters and palinopsia. New treatments were commenced in 14/40 (35%) patients. Of those, 6 (42%) were somewhat helpful: lamotrigine, diet/vitamin supplements/probiotics, lorazepam, cinnarizine, polarized glasses, chiropractic treatment. During follow up, 3 patients experienced new visual migraine aura without headache, and one had new migraine headache (total prevalence aura 35%, migraine 47.5%). There was no significant difference in anxiety and depression measured by the PHQ-8 and the GAD-7 questionnaire.
Conclusion: In a group of patients with VSS, symptoms can persist over 8 years without spontaneous resolution. New visual symptoms can develop, but visual snow itself might get less bothersome.
Disclosure: Nothing to disclose
Copyright © 2020 European Journal of Neurology
Feedback generates a second receptive field in neurons of the visual cortex
https://www.nature.com/articles/s41586-020-2319-4
Feedback generates a second receptive field in neurons of the visual cortex
Mirtazapine for treatment of visual snow syndrome (no effect on VSS, neither positive nor negative): A case series with insights into pathophysiology and therapy
https://journals.sagepub.com/doi/full/10.1177/2514183X20925695
https://pubmed.ncbi.nlm.nih.gov/30383334/
Mirtazapine for treatment of visual snow syndrome: A case series with insights into pathophysiology and therapy
Ozan Eren, Christoph J SchankinFirst Published May 20, 2020 Research Article
https://doi.org/10.1177/2514183X20925695
Article information
Open AccessCreative Commons Attribution, Non Commercial 4.0 License
Article Information
Volume: 4 issue: 1,
Article first published online: May 20, 2020; Issue published: January 1, 2020
Ozan Eren1, Christoph J Schankin2
1Department of Neurology, Ludwig Maximilians University Munich, University Hospital – Großhadern, Munich, Germany
2Department of Neurology, Inselspital, Bern University Hospital, University of Bern, Freiburgstrasse, Bern, Switzerland
Corresponding Author:
Christoph J Schankin, Department of Neurology, Inselspital, Bern University Hospital, University of Bern, Freiburgstrasse, CH-3010 Bern, Switzerland. Email: christoph.schankin@insel.ch
Conclusion
VSS keeps it secrets, and there is still no ideal medical approach. The best data exist for lamotrigine, which therefore could be discussed off-label with patients. Despite VSS having high impact on patients’ mood, antidepressants do not seem to be a solution for the visual symptoms. VSS deserves more attention, and we encourage physicians to not only present medications helpful but also the ones being unsuccessful to avoid unnecessary trials in other patients.
The Visual Snow Initiative releases the Visual Imagery Project (VIP): a 21-day online protocol investigating the use of customized visual imagery to reduce visual snow symptoms
Introducing The Visual Imagery Project
https://visualsnowproject.com/
The Visual Snow Initiative is excited to announce the release of the Visual Imagery Project (VIP), a 21-day online protocol designed to reduce visual snow symptoms via custom created visual imagery. Those who would like to participate can register now and begin your 21 day protocol. To begin, click here: visualsnowproject.com.
In order to get the full benefit of the Visual Imagery Project, we encourage you to watch both video tutorials.
Only desktops and laptops can be used for the VIP.
Only Google Chrome and Firefox browsers will work with the VIP.
These browsers are available for download free of charge on the VIP’s homepage.
The VIP’s protocol is 21 days and each session is approximately 30 minutes per day.
Each day, before beginning the viewing session, you will need to complete a Progress Evaluation. The information you provide will be saved daily in order to track your progress.
Due to the size of the visual imagery files used in the VIP, a strong WiFi connection is required. If you experience any technical difficulties with the Visual Imagery Project (VIP), please email us at info@visualsnowinitiative.org
VSI Research Team At Monash University Shares Impact Report
New research: “Visual snow requires a thorough ophthalmologic exam to exclude other ocular diseases”
https://www.ncbi.nlm.nih.gov/pubmed/32235228?dopt=Abstract
Visual snow requires a thorough ophthalmologic exam to exclude other ocular diseases.
Synaptic ribbons foster active zone stability and illumination-dependent active zone enrichment of RIM2 and Cav1.4 in photoreceptor synapses
https://www.nature.com/articles/s41598-020-62734-0
Synaptic ribbons foster active zone stability and illumination-dependent active zone enrichment of RIM2 and Cav1.4 in photoreceptor synapses
VIDEO: Structural and functional footprint of visual snow syndrome
Structural and functional footprint of visual snow syndrome
https://academic.oup.com/brain/advance-article/doi/10.1093/brain/awaa053/5811372
https://academic.oup.com/brain/article/143/4/1106/5811372
https://www.ncbi.nlm.nih.gov/pubmed/32211752?dopt=Abstract
TITLE:
Structural and functional footprint of visual snow syndrome.
DESCRIPTION:
Related Articles
Structural and functional footprint of visual snow syndrome.
Brain. 2020 Mar 24;:
Authors: Schankin CJ, Maniyar FH, Chou DE, Eller M, Sprenger T, Goadsby PJ
Abstract
Patients with visual snow syndrome suffer from a continuous pan-field visual disturbance, additional visual symptoms, tinnitus, and non-perceptional symptoms. The pathophysiology of visual symptoms might involve dysfunctional visual cortex. So far, the extra-visual system has not been investigated. We aimed at identifying structural and functional correlates for visual and non-visual symptoms in visual snow syndrome. Patients were compared to age- and sex-matched controls using 18F-2-fluoro-2-deoxy-d-glucose PET (n = 20 per group) and voxel-based morphometry (n = 17 per group). Guided by the PET results, region of interest analysis was done in voxel-based morphometry to identify structural-functional correspondence. Grey matter volume was assessed globally. Patients had corresponding hypermetabolism and cortical volume increase in the extrastriate visual cortex at the junction of the right lingual and fusiform gyrus. There was hypometabolism in the right superior temporal gyrus and the left inferior parietal lobule. Patients had grey matter volume increases in the temporal and limbic lobes and decrease in the superior temporal gyrus. The corresponding structural and functional alterations emphasize the relevance of the visual association cortex for visual snow syndrome. The broad structural and functional footprint, however, confirms the clinical impression that the disorder extends beyond the visual system.
PMID: 32211752 [PubMed – as supplied by publisher]
PMID:
PubMed:32211752
DATE FOUND:
03/27/20 03:26PM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/32211752?dopt=Abstract
Not All That Flickers Is Visual Snow
https://journals.lww.com/jneuro-ophthalmology/Abstract/publishahead/Not_All_That_Flickers_Is_Snow.99020.aspx
https://www.ncbi.nlm.nih.gov/pubmed/32235228?dopt=Abstract
TITLE:
Not All That Flickers Is Snow.
DESCRIPTION:
Related Articles
Not All That Flickers Is Snow.
J Neuroophthalmol. 2020 Mar 24;:
Authors: Patel RC, Vitale AT, Creel DJ, Digre KB
Abstract
A woman presented with bilateral visual disturbances that had been diagnosed as visual snow. Dilated ophthalmic examination and multimodal imaging were strongly suggestive of birdshot chorioretinopathy, meriting initiation of systemic immunomodulatory therapy. Visual snow requires a thorough ophthalmologic exam to exclude other ocular diseases.
PMID: 32235228 [PubMed – as supplied by publisher]
PMID:
PubMed:32235228
DATE FOUND:
04/03/20 06:02AM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/32235228?dopt=Abstract
Insular and occipital changes in visual snow syndrome: a BOLD fMRI and MRS study to investigate the pathophysiology of VS
https://onlinelibrary.wiley.com/doi/full/10.1002/acn3.50986
https://www.ncbi.nlm.nih.gov/pubmed/32154676?dopt=Abstract
TITLE:
Insular and occipital changes in visual snow syndrome: a BOLD fMRI and MRS study.
DESCRIPTION:
Insular and occipital changes in visual snow syndrome: a BOLD fMRI and MRS study.
Ann Clin Transl Neurol. 2020 Mar 10;:
Authors: Puledda F, Ffytche D, Lythgoe DJ, O’Daly O, Schankin C, Williams SCR, Goadsby PJ
Abstract
OBJECTIVE: To investigate the pathophysiology of visual snow (VS), through a combined functional neuroimaging and magnetic resonance spectroscopy (1 H-MRS) approach.
METHODS: We applied a functional MRI block-design protocol studying the responses to a visual stimulation mimicking VS, in combination with 1 H-MRS over the right lingual gyrus, in 24 patients with VS compared to an equal number of age- and gender-matched healthy controls.
RESULTS: We found reduced BOLD responses to the visual stimulus with respect to baseline in VS patients compared to controls, in the left (k = 291; P = 0.025; peak MNI coordinate [-34 12 -6]) and right (k = 100; P = 0.003; peak MNI coordinate [44 14 -2]) anterior insula. Our spectroscopy analysis revealed a significant increase in lactate concentrations in patients with respect to controls (0.66 ± 0.9 mmol/L vs. 0.07 ± 0.2 mmol/L; P < 0.001) in the right lingual gyrus. In this area, there was a significant negative correlation between lactate concentrations and BOLD responses to visual stimulation (P = 0.004; r = -0.42), which was dependent on belonging to the patient group. INTERPRETATION: As shown by our BOLD analysis, VS is characterized by a difference in bilateral insular responses to a visual stimulus mimicking VS itself, which could be due to disruptions within the salience network. Our results also suggest that patients with VS have a localized disturbance in extrastriate anaerobic metabolism, which may in turn cause a decreased metabolic reserve for the regular processing of visual stimuli. PMID: 32154676 [PubMed - as supplied by publisher] PMID: PubMed:32154676 DATE FOUND: 03/11/20 06:01AM LINK / URL: https://www.ncbi.nlm.nih.gov/pubmed/32154676?dopt=Abstract
Dynamic dot displays reveal material motion network in the human brain [Preprint]
https://www.biorxiv.org/content/10.1101/2020.03.09.983593v2.full
Dynamic dot displays reveal material motion network in the human brain
Current Observations on Visual Snow Syndrome by Dr. Owen White
Current Observations on Visual Snow Syndrome by Dr. Owen White
Current Observations on Visual Snow Syndrome by Dr. Owen White
Visual snow in hallucinogen-persisting perception disorder: a case report
https://pubmed.ncbi.nlm.nih.gov/32076839/
https://pubmed.ncbi.nlm.nih.gov/32076839-visual-snow-in-hallucinogen-persisting-perception-disorder/?dopt=Abstract
https://www.ncbi.nlm.nih.gov/pubmed/32076839?dopt=Abstract
https://link.springer.com/article/10.1007%2Fs00347-020-01056-y
TITLE:
[Visual snow in hallucinogen-persisting perception disorder].
DESCRIPTION:
Related Articles
Ophthalmologe. 2020 Feb 19;:
Authors: Schatten H, Eter N, Mihailovic N
Abstract
This article presents the case of a 24-year-old female patient who was referred to this department due to permanent flickering in front of both eyes. This flickering, described as being like visual snow in television, had started 1.5 years ago and was perceived to be very disturbing. Visual acuity, visual field and morphology of the anterior and posterior segment were bilaterally inconspicuous. A neurological examination including a magnetic resonance imaging of the cranium (cMRI) and visual evoked potentials (pattern-VEP) also showed no abnormalities. Furthermore, the patient suffered from schizophrenia. This also first occurred 1.5 years ago directly after consumption of a “narcotic cocktail” consisting of amphetamines, hallucinogens and alcohol. In a synopsis of the findings the patient was diagnosed with type II hallucinogen-persisting perception disorder. Treatment options for this disease are limited and the symptoms often remain permanently.
PMID: 32076839 [PubMed – as supplied by publisher]
PMID:
PubMed:32076839
DATE FOUND:
02/21/20 01:29PM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/32076839?dopt=Abstract
Shedding new light on visual snow syndrome
https://www.nature.com/articles/s41582-020-0324-8
https://www.ncbi.nlm.nih.gov/pubmed/32071423?dopt=Abstract
TITLE:
Shedding new light on visual snow syndrome.
DESCRIPTION:
Related Articles
Shedding new light on visual snow syndrome.
Nat Rev Neurol. 2020 Feb 18;:
Authors: Wood H
PMID: 32071423 [PubMed – as supplied by publisher]
PMID:
PubMed:32071423
DATE FOUND:
02/20/20 06:03AM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/32071423?dopt=Abstract
Additive effect of contrast and velocity suggests the role of strong excitatory drive in suppression of visual gamma response
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0228937
Additive effect of contrast and velocity suggests the role of strong excitatory drive in suppression of visual gamma response
Visual snow syndrome: a review on diagnosis, pathophysiology, and treatment
https://journals.lww.com/co-neurology/Abstract/2020/02000/Visual_snow_syndrome__a_review_on_diagnosis,.13.aspx
https://europepmc.org/article/med/31714263
Visual snow syndrome: a review on diagnosis, pathophysiology, and treatment.
Prevalence of visual snow syndrome in the UK is around 2%
https://onlinelibrary.wiley.com/doi/abs/10.1111/ene.14150
https://www.ncbi.nlm.nih.gov/pubmed/31999855?dopt=Abstract
Prevalence of visual snow syndrome in the UK is around 2%
TITLE:
Prevalence of visual snow syndrome in the UK.
DESCRIPTION:
Prevalence of visual snow syndrome in the UK.
Eur J Neurol. 2020 Jan 30;:
Authors: Kondziella D, Olsen MH, Dreier JP
Abstract
BACKGROUND: Visual snow syndrome is a recently described condition of unknown prevalence. We investigated the prevalence in a representative population sample from the UK and tested the hypothesis that visual snow syndrome is associated with young age, headache, tinnitus and mood impairment.
METHODS: Using a crowdsourcing platform, we recruited a representative sample of 1015 adult laypeople from the UK, matched for age, gender and ethnicity according to national census data. Participants were unprimed, i.e. were inquired about the “frequency of certain medical conditions” but not “visual snow syndrome”.
RESULTS: Thirty-eight of 1015 participants reported symptoms compatible with visual snow (3.7%, 95% CI 2.7-5.2), and 22/1015 met criteria for visual snow syndrome (2.2%, 95% CI 1.4-3.3). Female-to-male ratio for visual snow syndrome was 1.6:1. Subjects with visual snow syndrome were older (50.6 ±14 years) than the population mean (44.8 ±15 years), albeit not statistically different (p=0.06). Of 22 participants with visual snow syndrome, 16 had mood symptoms (72.7%; p=0.01), 13 had headache (54.5%, p=0.06), including 5 with visual migraine aura (22.7%, p=0.15), and 13 had tinnitus (59.1%, p<0.001). No participant had diabetes or a cleft lip (control questions). Following a multivariable regression analysis to adjust for age and gender, only the association between visual snow syndrome and tinnitus remained significant (OR 3.93, 95% CI 1.63-9.9; p=0.003). CONCLUSIONS: The UK prevalence of visual snow syndrome is around 2%. We confirmed an association with tinnitus, but unprimed laypeople with visual snow syndrome are on average older than those seeking medical attention. PMID: 31999855 [PubMed - as supplied by publisher] PMID: PubMed:31999855 DATE FOUND: 01/31/20 06:02AM LINK / URL: https://www.ncbi.nlm.nih.gov/pubmed/31999855?dopt=Abstract
Visual Snow is Real — and migraine, tinnitus are frequent comorbidities
https://www.medpagetoday.com/neurology/generalneurology/84531
Visual Snow is Real
— Migraine, tinnitus are frequent comorbidities
by Judy George, Senior Staff Writer, MedPage Today January 24, 2020
Visual Snow: Are We Beginning to See the Light? [Editorial]
https://n.neurology.org/content/early/2020/01/16/WNL.0000000000008913
https://pubmed.ncbi.nlm.nih.gov/31949088-visual-snow-are-we-beginning-to-see-the-light/
Visual Snow: Are We Beginning to See the Light?
Visual snow syndrome: A clinical and phenotypical description of 1,100 cases
https://n.neurology.org/content/early/2020/01/15/WNL.0000000000008909
https://www.ncbi.nlm.nih.gov/pubmed/31941797?dopt=Abstract
TITLE:
Visual snow syndrome: A clinical and phenotypical description of 1,100 cases.
DESCRIPTION:
Related Articles
Visual snow syndrome: A clinical and phenotypical description of 1,100 cases.
Neurology. 2020 Jan 15;:
Authors: Puledda F, Schankin C, Goadsby PJ
Abstract
OBJECTIVE: To validate the current criteria of visual snow and to describe its common phenotype using a substantial clinical database.
METHODS: We performed a web-based survey of patients with self-assessed visual snow (n = 1,104), with either the complete visual snow syndrome (n = 1,061) or visual snow without the syndrome (n = 43). We also describe a population of patients (n = 70) with possible hallucinogen persisting perception disorder who presented clinically with visual snow syndrome.
RESULTS: The visual snow population had an average age of 29 years and had no sex prevalence. The disorder usually started in early life, and ≈40% of patients had symptoms for as long as they could remember. The most commonly experienced static was black and white. Floaters, afterimages, and photophobia were the most reported additional visual symptoms. A latent class analysis showed that visual snow does not present with specific clinical endophenotypes. Severity can be classified by the amount of visual symptoms experienced. Migraine and tinnitus had a very high prevalence and were independently associated with a more severe presentation of the syndrome.
CONCLUSIONS: Clinical characteristics of visual snow did not differ from the previous cohort in the literature, supporting validity of the current criteria. Visual snow likely represents a clinical continuum, with different degrees of severity. On the severe end of the spectrum, it is more likely to present with its common comorbid conditions, migraine and tinnitus. Visual snow does not depend on the effect of psychotropic substances on the brain.
PMID: 31941797 [PubMed – as supplied by publisher]
PMID:
PubMed:31941797
DATE FOUND:
01/17/20 04:38PM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/31941797?dopt=Abstract
Elucidating the pathophysiological signature of visual snow
https://research.monash.edu/en/projects/elucidating-the-pathophysiological-signature-of-visual-snow
Elucidating the pathophysiological signature of visual snow
Fielding, Joanne (Primary Chief Investigator (PCI))White, Owen (Chief Investigator (CI))
Department of Neuroscience
Project: Research
Quantification of photophobia in visual snow syndrome: A case-control study
https://journals.sagepub.com/doi/abs/10.1177/0333102419896780?journalCode=cepa
https://pubmed.ncbi.nlm.nih.gov/31865761-quantification-of-photophobia-in-visual-snow-syndrome-a-case-control-study/
Quantification of photophobia in visual snow syndrome: A case-control study
Article first published online: December 22, 2019
Ozan E Eren1, Ruth Ruscheweyh1, Andreas Straube1, Christoph J Schankin1, 2
Department of Neurology, Ludwig Maximilians University Munich, University Hospital – Großhadern, Munich, Germany
Department of Neurology, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland
Corresponding Author:
Christoph J Schankin, Department of Neurology, Inselspital, Bern University Hospital, University of Bern, Freiburgstrasse, CH-3010 Bern, Switzerland. Email: christoph.schankin@insel.ch
Abstract
Objective
To quantify photophobia in visual snow syndrome (VSS), a debilitating migraine-associated visual disturbance manifesting with continuous “TV snow-like” flickering dots in the entire visual field and additional visual symptoms, such as photophobia.
Methods
Photophobia was compared between 19 patients with VSS and 19 controls matched for age, sex, migraine and aura using the Leiden Visual Sensitivity Scale (L-VISS).
Results
Patients with VSS had an increased L-VISS-score compared to matched controls [(22.2 ± 5.9 vs. 4.4 ± 4.8; ANOVA, factors VSS and comorbid migraine: Main effect for VSS (F = 100.70; p < 0.001), but not for migraine (F < 0.01; p = 1.00) or the interaction (F = 1.93; p = 0.16)]. An L-VISS-score of 14 identified VSS with a sensitivity and specificity of 95% (Receiver Operating Characteristic analysis, 0.986 ± 0.014, p ≤ 0.001).
Conclusion
Patients with VSS suffer continuously from photophobia at a level similar to chronic migraineurs during attacks. Although migraine and VSS share dysfunctional visual processing, patients with VSS might be more severely affected.
Keywords Visual sensitivity, migraine, aura, visual processing
New clinical trial to treat patients with debilitating symptoms of visual snow (VS)
Until recently, a search for “visual snow” on ClinicalTrials.gov would return no results (“No Studies Found”).
There were ZERO clinical trials that focused on treating or managing visual snow syndrome or its symptoms.
But that is no longer the case.
Finally… the First Ever Visual Snow Clinical Trial
There is finally a clinical trial that is designed to “to treat patients with debilitating symptoms of visual snow (VS)” and it will begin recruiting patients soon.
It was added to the official clinical trials database on December 4, 2019.
Here is the link:
https://clinicaltrials.gov/ct2/show/NCT04184726
Here is an excerpt:
For this study, the investigators will assess the use of MBCT-vision in patients with visual snow or associated visual symptoms, migrainous visual aura or photophobia.
Is there a catch?
The only issue, which some people might find discouraging, is the type of treatment being offered in this clinical trial…
Sadly, it is NOT a drug or a procedure or what you might consider a potential cure.
Instead, the treatment is a mindfulness-based intervention called Mindfulness-Based Cognitive Therapy (MCBT).
And although it might not be the miracle you’ve been waiting for, consider the bright side…
This is the first ever interventional clinical trial that specifically addresses visual snow syndrome and its associated symptoms. And that is a HUGE milestone and a step in the right direction. (Think of this first ever VS clinical trial as a stepping stone toward more awareness, more research funding, and hopefully more exciting clinical trials.)
More to follow?
Can we expect more visual snow clinical trials to follow? Time will tell. Check the front page regularly for more updates, or…
For the latest visual snow treatment-related news and information – including clinical trial alerts – subscribe to the newsletter. These once-weekly email updates will begin sending soon.
Imaging the Visual Network in the Migraine Spectrum: possible hypotheses on the underlying pathophysiology of visual snow
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6923266/#s7title
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6923266/
https://www.frontiersin.org/articles/10.3389/fneur.2019.01325/full
https://www.ncbi.nlm.nih.gov/pubmed/31920945?dopt=Abstract
TITLE:
Imaging the Visual Network in the Migraine Spectrum.
DESCRIPTION:
Related Articles
Imaging the Visual Network in the Migraine Spectrum.
Front Neurol. 2019;10:1325
Authors: Puledda F, Ffytche D, O’Daly O, Goadsby PJ
Abstract
The involvement of the visual network in migraine pathophysiology has been well-known for more than a century. Not only is the aura phenomenon linked to cortical alterations primarily localized in the visual cortex; but also migraine without aura has shown distinct dysfunction of visual processing in several studies in the past. Further, the study of photophobia, a hallmark migraine symptom, has allowed unraveling of distinct connections that link retinal pathways to the trigeminovascular system. Finally, visual snow, a recently recognized neurological disorder characterized by a continuous visual disturbance, is highly comorbid with migraine and possibly shares with it some common pathophysiological mechanisms. Here, we review the most relevant neuroimaging literature to date, considering studies that have either attempted to investigate the visual network or have indirectly shown visual processing dysfunctions in migraine. We do this by taking into account the broader spectrum of migrainous biology, thus analyzing migraine both with and without aura, focusing on light sensitivity as the most relevant visual symptom in migraine, and finally analyzing the visual snow syndrome. We also present possible hypotheses on the underlying pathophysiology of visual snow, for which very little is currently known.
PMID: 31920945 [PubMed]
PMID:
PubMed:31920945
DATE FOUND:
01/11/20 06:04AM
LINK / URL:
https://www.ncbi.nlm.nih.gov/pubmed/31920945?dopt=Abstract
For Those Waiting for the Visual Snow Initiative’s Project (VIP) Launch
For Those Waiting for the Visual Snow Initiatives Project (VIP) Launch
For Those Waiting for the Visual Snow Initiatives Project (VIP) Launch
Pediatric Visual Snow Syndrome (VSS): A Case Series
https://pubs.covd.org/VDR/issue5-4/?page=37
https://www.researchgate.net/profile/Barry_Tannen/publication/338185435_Pediatric_Visual_Snow_Syndrome_VSS_A_Case_Series/links/5e0f7d0a299bf10bc38f1989/Pediatric-Visual-Snow-Syndrome-VSS-A-Case-Series.pdf
Pediatric Visual Snow Syndrome (VSS): A Case Series
Kenneth J. Ciuffreda, OD, PhD1
M.H. Esther Han, OD
Barry Tannen, OD
SUNY/College of Optometry
Brain Injury Clinical Research Unit
New York, New York
neuro-optometric, therapeutic interventions, namely tinted spectacles and oculomotor-based vision therapy
Episodic Visual Snow Associated With Migraine Attacks
https://jamanetwork.com/journals/jamaneurology/article-abstract/2755346
https://www.ncbi.nlm.nih.gov/pubmed/31764944?dopt=Abstract
Episodic Visual Snow Associated With Migraine Attacks.
JAMA Neurol
Related Articles
Episodic Visual Snow Associated With Migraine Attacks.
JAMA Neurol. 2019 Nov 25;:
Authors: Hodak J, Fischer U, Bassetti CLA, Schankin CJ
PMID: 31764944 [PubMed – as supplied by publisher]
PubMed:31764944
Colorimetric Intervention for Visual Snow Syndrome (VSS) Following Brain Surgery
https://www.aaopt.org/detail/knowledge-base-article/colorimetric-intervention-for-visual-snow-syndrome-vss-following-brain-surgery-339197-3224879
Colorimetric Intervention for Visual Snow Syndrome (VSS) Following Brain Surgery
M.H. Esther Han
Colorimetric intervention was found to be successful in a patient with the rare condition of VSS. Her VSS perceptual symptoms reduced, and she reads more comfortably for longer durations, with the specific custom Cerium tinted spectacles.
Hallucinogen persisting perception disorder: A literature review and three case reports
https://www.tandfonline.com/doi/abs/10.1080/10550887.2019.1673655?journalCode=wjad20
https://www.ncbi.nlm.nih.gov/pubmed/31613183
Hallucinogen persisting perception disorder: A literature review and three case reports
Functionally Distinct Gamma Range Activity Revealed by Stimulus Tuning in Human Visual Cortex
https://www.cell.com/current-biology/fulltext/S0960-9822(19)31020-6
Functionally Distinct Gamma Range Activity Revealed by Stimulus Tuning in Human Visual Cortex
No Studies found for: Visual Snow (October 3, 2019)
https://clinicaltrials.gov/ct2/results?cond=Visual+Snow&term=&cntry=&state=&city=&dist=
No Studies found for: Visual Snow (September 2, 2019)
https://clinicaltrials.gov/ct2/results?cond=Visual+Snow&term=&cntry=&state=&city=&dist=
No Studies found for: Visual Snow (September 2, 2019)
Symptoms related to the visual system in migraine
https://f1000research.com/articles/8-1219/v1
https://www.ncbi.nlm.nih.gov/pubmed/31448081?dopt=Abstract
Symptoms related to the visual system in migraine.
F1000Res
Related Articles
Symptoms related to the visual system in migraine.
F1000Res. 2019;8:
Authors: van Dongen RM, Haan J
Abstract
Migraine is a common headache disorder characterized by often-severe headaches that may be preceded or accompanied by a variety of visual symptoms. Although a typical migraine aura is not difficult to diagnose, patients with migraine may report several other visual symptoms, such as prolonged or otherwise atypical auras, “visual blurring”, “retinal migraine”, “ophthalmoplegic migraine”, photophobia, palinopsia, and “visual snow”. Here, we provide a short overview of these symptoms and what is known about the relationship with migraine pathophysiology. For some symptoms, the association with migraine is still debated; for other symptoms, recent studies indicate that migraine mechanisms play a role.
PMID: 31448081 [PubMed – in process]
PubMed:31448081
Prestimulus feedback connectivity biases the content of visual experiences
https://www.pnas.org/content/116/32/16056
Prestimulus feedback connectivity biases the content of visual experiences
No Studies found for: Visual Snow (July 7, 2019)
https://clinicaltrials.gov/ct2/results?cond=Visual+Snow&term=&cntry=&state=&city=&dist=
Novel clinical features of glycine receptor antibody syndrome, including visual snow
https://nn.neurology.org/content/6/5/e592
https://www.ncbi.nlm.nih.gov/pubmed/31355325?dopt=Abstract
Novel clinical features of glycine receptor antibody syndrome: A series of 17 cases.
Neurol Neuroimmunol Neuroinflamm
Novel clinical features of glycine receptor antibody syndrome: A series of 17 cases.
Neurol Neuroimmunol Neuroinflamm. 2019 Sep;6(5):e592
Authors: Piquet AL, Khan M, Warner JEA, Wicklund MP, Bennett JL, Leehey MA, Seeberger L, Schreiner TL, Paz Soldan MM, Clardy SL
Abstract
Objective: To describe novel clinical features of GlyRα1-IgG-positive patients.
Methods: Patients with a positive serum GlyRα1-IgG were identified during a 2-year period from July 2016 to December 2018 at 2 academic centers and followed prospectively. All patients in this series were evaluated in the Neuroimmunology and Autoimmune Neurology clinics at the University of Utah or the University of Colorado.
Results: Thirteen of 17 patients had phenotypes more typically associated with glutamic acid decarboxylase (GAD65) antibody syndromes, consisting of stiff-person syndrome (SPS) with parkinsonism or cerebellar signs. One patient with parkinsonism had a presentation similar to rapidly progressive multiple system atrophy with severe dysautonomia. Ten of 17 patients had various visual symptoms including visual snow, spider web-like images forming shapes and 3-dimensional images, palinopsia, photophobia, visual hallucinations, synesthesia, and intermittent diplopia. Three of 17 patients presented with primarily autoimmune epilepsy accompanied by psychiatric symptoms.
Conclusions: Clinicians should consider testing for GlyR antibodies in GAD65 antibody-negative or low-positive GAD65 antibody patients with SPS-like presentations, especially in the setting of atypical features such as visual disturbances, parkinsonism, or epilepsy.
PMID: 31355325 [PubMed – in process]
PubMed:31355325
Study: For some patients with visual snow, lamotrigine resulted in partial remission of symptoms
https://www.ncbi.nlm.nih.gov/pubmed/31213497
https://n.neurology.org/content/early/2019/06/18/WNL.0000000000007825
No Studies found for: Visual Snow (June 21, 2019)
https://clinicaltrials.gov/ct2/results?cond=Visual+Snow&term=&cntry=&state=&city=&dist=
Treatment effects and comorbid diseases in 58 patients with visual snow
https://n.neurology.org/content/early/2019/06/18/WNL.0000000000007825
https://www.ncbi.nlm.nih.gov/pubmed/31213497?dopt=Abstract
Treatment effects and comorbid diseases in 58 patients with visual snow.
Neurology
Related Articles
Treatment effects and comorbid diseases in 58 patients with visual snow.
Neurology. 2019 Jun 18;:
Authors: van Dongen RM, Waaijer LC, Onderwater GLJ, Ferrari MD, Terwindt GM
Abstract
OBJECTIVE: To evaluate pharmacologic treatment options for visual snow and to report prevalence of comorbid diseases.
METHODS: Medical charts of patients with a diagnosis of visual snow at the neurology outpatient clinic were reviewed on prescribed medication, and comorbid migraine, tinnitus, and psychiatric conditions including depression and anxiety.
RESULTS: From 2007 to 2018, 58 patients were diagnosed with visual snow. Comorbid migraine was present in 51.7% of patients, lifetime depression in 41.4%, and lifetime anxiety in 44.8%. Lamotrigine was prescribed most frequently (26/58) and resulted in partial remission of symptoms in 5/26 (19.2%). No patients reported complete remission. Adverse events occurred in 13/26 (50.0%) patients. None of the other prescribed drugs (valproate [n = 7], topiramate [n = 4], acetazolamide [n = 2], flunarizine [n = 1]) led to improvement except for topiramate in one patient, who discontinued, however, because of adverse events.
CONCLUSIONS: Of medication prescribed (lamotrigine, valproate, acetazolamide, flunarizine), only lamotrigine afforded some improvement in a small minority of patients. Migraine, depression, anxiety, and tinnitus were common comorbid diseases.
CLASSIFICATION OF EVIDENCE: This study provides Class IV evidence that for some patients with visual snow, lamotrigine resulted in partial remission of symptoms.
PMID: 31213497 [PubMed – as supplied by publisher]
PubMed:31213497
Tracking functional and structural brain plasticity in patients with visual snow
https://ww5.aievolution.com/hbm1901/index.cfm?do=abs.viewAbs&abs=2590
Tracking functional and structural brain plasticity in patients with visual snow